How Does Semaglutide Work?
Semaglutide has become a popular topic around modern weight management, and for good reason. Backed by strong clinical data and used under medical supervision, semaglutides are helping many patients achieve meaningful, sustainable weight loss while improving overall metabolic health.
This article explains how semaglutides work, what they do inside the body, and what patients should realistically expect. We’ll also cut through the noise with a clear Myths vs. Facts section, so you can separate credible medical guidance from social media hype.
If you’re exploring semaglutide for weight loss Charleston options, this guide will give you the foundational knowledge you need before starting a conversation with a provider.
What Is Semaglutide?
Semaglutide is a medication that belongs to a class of drugs called GLP-1 receptor agonists. GLP-1 stands for glucagon-like peptide-1, a hormone your body naturally releases after eating.
Originally developed to help manage type 2 diabetes, semaglutide was later found to have a powerful secondary effect: significant weight loss. This led to its expanded use in medically supervised weight management programs.
Semaglutide is not a stimulant, crash diet, and or osmetic shortcut. It works by addressing the biological drivers of appetite, hunger, and blood sugar regulation.
How Does Semaglutide Work in the Body?
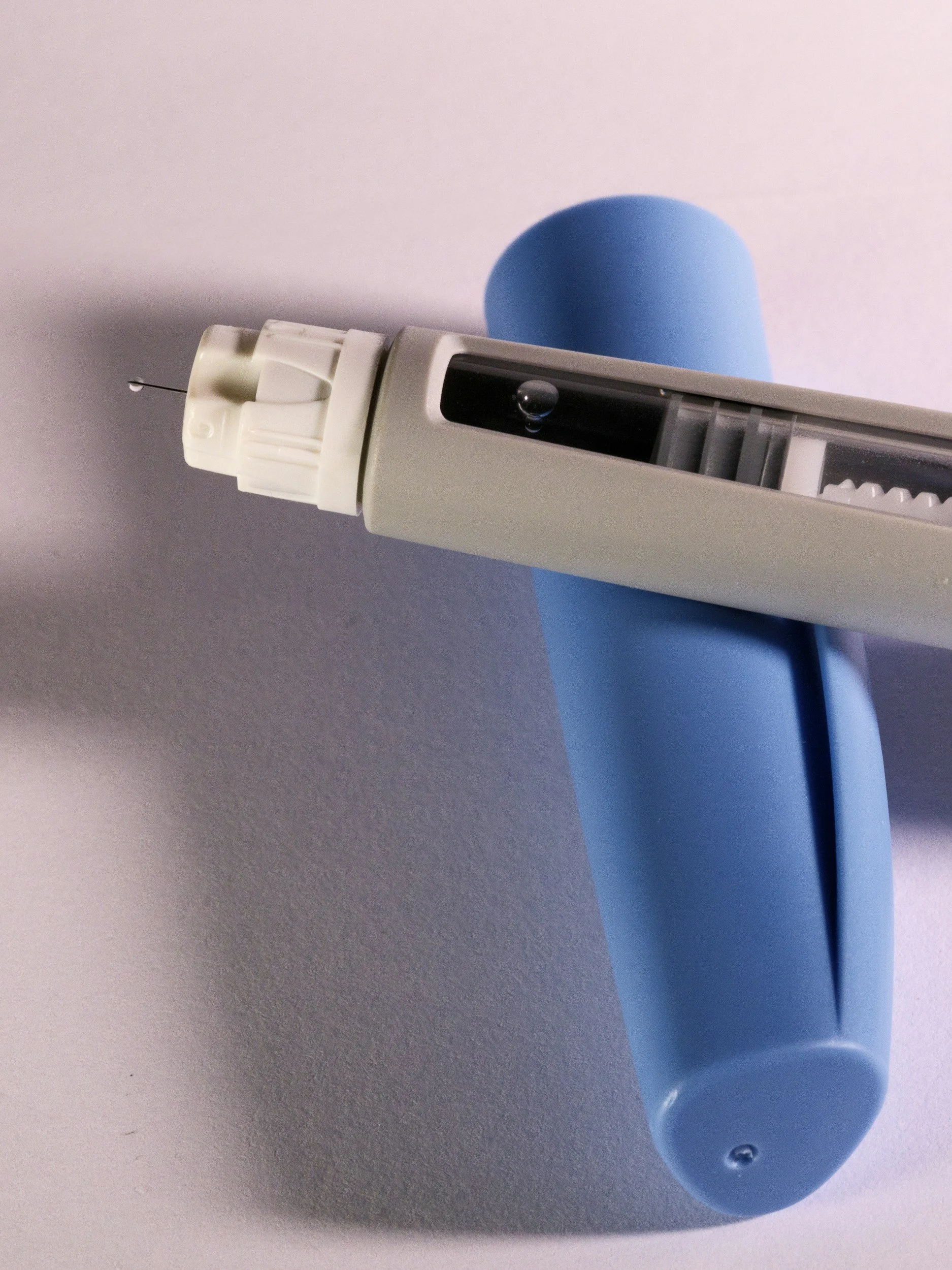
If you’re looking for somewhere nearby to start semaglutide, it’s important to understand how it works in the body. Semaglutide support weight loss through three primary physiological mechanisms:
1. Appetite Regulation in the Brain
Semaglutide acts on GLP-1 receptors in the brain, specifically areas involved in appetite and satiety.
What this means in practical terms:
You feel full sooner
You stay full longer
Food noise and cravings are reduced
2. Slowed Gastric Emptying
Semaglutide slows how quickly food leaves the stomach. This leads to:
Longer-lasting fullness after meals
Fewer spikes in hunger between meals
Reduced portion sizes without forced restriction
This effect is one reason gradual dose titration is important. Too much too fast can increase side effects like nausea.
3. Improved Blood Sugar and Insulin Response
Semaglutide improves how the body handles glucose by:
Enhancing insulin release when blood sugar rises
Reducing glucagon (a hormone that raises blood sugar)
Even for patients without diabetes, this stabilization can reduce energy crashes, cravings, and fat storage signals tied to insulin resistance.
Why Semaglutides Support Sustainable Weight Loss
Traditional diets often fail because they fight biology. Semaglutides work with it.
By reducing hunger signals and improving metabolic efficiency, semaglutide helps patients:
Maintain a calorie deficit without extreme restriction
Avoid the binge/restrict cycle
Preserve consistency over months, not weeks
This is why semaglutide is most effective when paired with medical oversight, nutritional guidance, and long-term planning, not quick fixes.
Myths vs. Facts About Semaglutide
Myth 1: Semaglutide Is “Cheating”
Fact: Obesity is a chronic medical condition influenced by hormones, genetics, and metabolism. Treating it medically is no different than treating hypertension or diabetes.
Myth 2: You’ll Gain All the Weight Back
Fact: Weight regain is linked to stopping treatment without lifestyle support. Under medical guidance, patients learn sustainable habits that support long-term success, even if medication is adjusted later.
Myth 3: Semaglutide Works Instantly
Fact: Healthy, lasting weight loss is gradual. Most patients see steady progress over weeks to months, not overnight changes.
Myth 4: Side Effects Are Severe for Everyone
Fact: Most side effects are mild and temporary, often during dose increases. Proper titration and medical supervision significantly reduce issues like nausea or GI discomfort.
Myth 5: Anyone Can Take Semaglutide
Fact: Semaglutide is not appropriate for everyone. A medical evaluation is essential to assess safety, medications, and health history.
Who Is a Good Candidate for Semaglutide?
Semaglutide may be appropriate for adults who:
Struggle with weight despite diet and exercise
Experience frequent hunger or cravings
Have insulin resistance or metabolic challenges
Want a medically supervised, sustainable approach
A provider should always evaluate:
BMI and weight history
Medical conditions
Current medications
Long-term goals
This is where personalized care matters.
Semaglutide Available Through Holy City Med
At Holy City Med, weight loss care is built around accessibility, transparency, and patient-first medicine.
Instead of navigating insurance complexity, patients can access care through a simple medical membership model that includes:
Direct access to providers
Clear pricing with no surprise bills
In-person visits, urgent care, and telehealth
Ongoing support, not one-off prescriptions
For patients searching for semaglutide nearby, Holy City Med offers a local, medically guided path that prioritizes safety and long-term outcomes, not trends.
Why Medical Supervision Matters
Semaglutide is powerful, but it’s not plug-and-play. Medical supervision ensures:
Proper dosing and titration
Monitoring for side effects
Adjustments based on progress
Integration with nutrition and lifestyle care
This approach reduces risk and dramatically improves results.
Experience Care Your Way
Whether you’re looking for a Primary Care doctor in Charleston, SC, accessible Urgent Care, or structured weight management support, Holy City Med delivers healthcare designed around real life, not insurance paperwork.
If you’re considering semaglutide and want credible guidance from a team that puts patients first, becoming a member gives you direct, affordable access to care when you need it.
Healthcare should be simple, effective, and human.